İlker Büyükyavuz, Saniye Ekinci, Arbay Özden Çiftçi, İbrahim Karnak, Mehmet Emin Şenocak, Feridun Cahit Tanyel, Nebil Büyükpamukçu
Department of Pediatric Surgery, Hacettepe University Faculty of Medicine, Ankara, Turkey
SUMMARY: Büyükyavuz İ, Ekinci S, Çiftçi AÖ, Karnak İ, Şenocak ME, Tanyel FC, Büyükpamukçu N. A retrospective study of choledochal cyst: clinical presentation, diagnosis and treatment. Turk J Pediatr 2003; 45: 321-325
The treatment and early diagnosis of choledochal cyst are very important to prevent complications of the disease. Delay in treatment can cause lethal complications like biliary cirrhosis and increased morbidity in patients.
We studied 26 children with choledochal cyst retrospectively for their clinical presentation, and for the diagnostic tools and treatment modalities, used.
The most common findings of choledochal cyst in our series were abdominal pain, vomiting, and ictures in contrast to the classical triad of the disease of jaundice, mass and pain. The most useful diagnostic tool was abdominal ultrasonography.
For the treatment, we preferred Roux-en-Y hepaticojejunostomy to the internal drainage procedures, and the results were excellent with minimal mortality and morbidity. We underline prompt diagnosis and treatment to prevent late complications of the disease.
Key words: choledochal cyst, biliary tract, jaundice, hepaticojejunostomy.
The choledochal cyst is the dilatation of either intra or extrahepatic biliary system or both. It was first described in 1852 by Douglas1-4.
Diagnostic and therapeutic applications for the choledochal cyst have changed quickly in the last decades. After reports of malignant tumors and biliary cirrhosis due to choledochal cyst, its management has increased in importance for the surgeons5.
Here, we report 26 cases of choledochal cyst with the diagnostic, therapeutic, and long-term results.
Material and Methods
Between 1984 and 2002, 26 children with choledochal cyst were recorded retrospectively for their age; gender; presenting clinical symptoms; physical, laboratory and histological findings; diagnostic methods; and operative procedures.
Todani’s classification was used for the determination of the cyst type6.
Ultrasonography (USG), scintigraphy, computerized tomography (CT), percutaneous transhepatic cholangiography (PTC), oral and
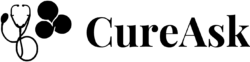
intravenous cholecystography, and magnetic resonance (MR) cholangiography were used as diagnostic tools (Fig 1-2).
Follow-up features of the patients were recorded from one month to six years.
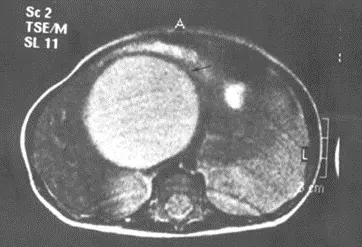
Fig. 1. The choledochal cyst (thin arrow) demonstrated with magnetic resonance imaging cholangiography.
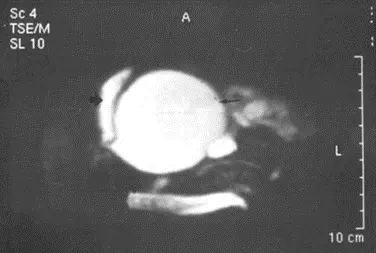
Fig. 2. The choledochal cyst (thin arrow) and gallbladder (thick arrow) demonstrated with magnetic resonance imaging cholangiography.
Fig. 3. Abdominal computerized tomography (CT) showing showing the choledochal cyst (thin arrow).
Results
Of the 26 patients with choledochal cyst, seven of the cases were male (27%); female to male ratio was 2.7:1, Five patients were less than one year of age, and all patients were less than14 years of age at the time of operation. The mean age of the patients at presentation was 5.8±4.2 (mean±standard deviation) years.
Presenting symptoms varied among the patients; however, the most common symptoms were abdominal pain (n=20), and vomiting (n=16). Other symptoms including nausea (n=5), fever (n=8), acholic stool (n=7), distention (n=1), dysuria (n=1), diarrhea (n=1), and constipation (n=1) were rare, and only one patient was seen with the complaint of abdominal mass. The most frequent physical findings are tenderness of the right upper abdominal quadrant (n=10), intermittent jaundice (n=9), and hepatomegaly (n=8). Two patients presented the clinical picture of acute abdomen. Only five patients had palpable mass or fullness, and two patients had splenomegaly. Physical examination findings were completely normal in six patients. As a radiologic procedure, USG was used in all patients, and it detected choledochal cyst in patients, and suspected choledochal cyst in six. However, with USG, one patient was incorrectly diagnosed as hematoma, and another as hydatid cyst. USG showed lithiasis in gallbladder and in the cyst in three cases. Abdominal CT was used and showed choledochal cyst in two cases (Fig. 3). Preoperative scintigraphy was performed in eight patients, and detected choledochal cyst in two, suspected in three, and a disease other than choledochal cyst in three patients. Postoperative scintigraphy was done in three patients, and was normal. PTC was performed in one patient, and was diagnostic. Oral and intravenous cholangiography showed the choledochal cyst in four patients.
Laboratory findings demonstrated hemoglobin, thrombocyte, and blood coagulation parameters as normal. White blood cell count was elevated in five patients. Blood chemistry results showed minimal increase in alkaline phosphatase ALP (n=6), in aspartate transaminase (AST) (n=7), in gamma glutamyl transferase (GGT) (n=7), and in alanine transaminase (ALT) (n=7), and a much greater increase in ALP (n=2), in AST (n=5), in ALT (n=5), and in GGT (n=4). Bilirubin levels were increased in 11 patients, and only minimal elevation was seen in four patients. In five cases, albumin was decreased at admission. Blood amylase levels were controlled in 14 patients, and found elevated in two.
In 19 patients, accurate diagnosis was made before the operation; differential diagnosis with pancreatic pseudocyst could not be made in two. Biliary atresia (n=2), hydatid cyst (n=1), cystic mass (n=1), and hematoma following appendectomy (n=1) were the preoperative diagnoses in five patients before the operation. Type I cyst was found in 25 patients and type II in one. One patient died on the postoperative fifth day due to hepatic failure. Two patients had rupture of choledochal cyst on admission to hospital. Surgical procedures performed in the series included: total cystectomy + Roux-en-Y hepaticojejunostomy (n=20), cystoduodenostomy (n=3), cystojejunostomy (n=1), total cystectomy+hepaticoduodenostomy (n=1), and choledochoileostomy (n=1). Transduodenal sphincteroplasty had been performed in one patient in another clinic. Because of persistence of the cyst, we performed cystectomy and Roux-en-Y hepaticojejunostomy on this patient.
The mean duration of drains was 6.92±4.37 days. Broad-spectrum antibiotics with triple combination were given to the patients. Double antibiotic combinations in two, and second generation cephalosporin alone in one patient were used. The mean duration of antibiotics given was 8.56±5 days. The meantime of initiation of oral intake was 4.75±0.94 days, and of discharge was 10.56±5.82 days.
Peroperative liver biopsy was performed in 16 patients, and periportal fibrosis was found in two and cirrhotic changes in one. Biopsy results also showed metaplasia (n=1), atrophic changes (n=1), hyperplastic cylindirical epithelia (n=1), and islands of squamous cell (n=1) in cyst wall. In one patient, polyps in gallbladder were detected, and adenomyomatosis of gallbladder in another. Reoperation was needed for three patients: two for persisting cyst, and one for hemorrhage on the same day of first operation. During two months to six years of follow-up, three patients had an adhesive intestinal obstruction, which was managed by medical therapy in two. The third patient underwent adhesiolysis for the intestinal obstruction. Three patients did not come to the follow-up examinations, and the remainder had no complications.
Discussion
The incidence of choledochal cysts was reported to be less than 1 in 13,000-2 million patients, but they are now diagnosed more frequently with the aid of improved diagnostic techniques. The Oriental race seems to be affected more than others7.
There are some theories for the etiology of choledochal cyst. The widely accepted theory states that there is an inequality in proliferation of epithelial cells when the hepatic bud lumen is still occluded. Canalization of the bile ducts results in an abnormal dilated portion at the site of more active cellular proliferation and relatively weak walls. Hypoproliferation of the distal portion of the duct creates a relatively stenotic distal duct. Other theories suggest it to be congenital or acquired, due e to abnormal pancreaticobiliary duct junction or primary weakness of bile duct. However, the etiology of choledochal cyst remains unknown8-10.
Female predominance (around 75%) is shown in many reports of choledochal cyst, and our report proved this (73% female predominance).
Choledochal cysts are known primarily as a disease of young adults and children, since 60% of the patients are under the age of 10 years. We found 84% of our cases were 10 years of age or younger11.
The classical triad of jaundice, mass, and pain is considered as the most common and significant findings in the diagnosis of the choledochal cyst, especially in infancy. Suprisingly, no patient showed this triad in our series even in infancy. We found the most common presenting findings of patients to be abdominal pain and vomiting (58%). Contrary to the classical triad of the disease, the triad of abdominal pain, vomiting, and icterus was the most significant finding in our series (27%). During infancy, the most common finding was jaundice (83%), and jaundice with hepatomegaly (67%). Vomiting is known to occur following cyst infection or obstruction of the duodenum. Our records showed 60% vomiting without the above-mentioned symptoms12,13.
Abdominal USG and CT are both commonly used to demonstrate choledochal cyst even in the fetus during the prenatal period. Before the common use of USG to diagnose choledochal cyst, PTC and endoscopic retrograde cholangio- pancreaticography were definitive tests with 80-90% diagnostic accuracy14-16. We support the use of abdominal USG with 70% accuracy. This rate reached 92% with suspicion of the disease. Advancement in sonographic techniques and surgical procedures for the diagnosis and treatment helped us to handle choledochal cyst with minimal mortality and morbidity. It also decreased the rate of the pre-and post-operative complications.
Percutaneous transhepatic cholangiography was performed in only one patient, and it was diagnostic. Oral and intravenous cholangiography were made in four patients, and they were 100% diagnostic in contrast to the previous series11. A 99m Tc-HIDA radionuclide scan may show delayed filling of the abnormal biliary tree with contrast persisting in the cyst on the late images. Postoperative scan can also verify the patency of the anastomosis. Two of eight patients were diagnosed as choledochal cyst before surgery with the aid of scintigraphy in our series. Postoperative scintigraphy was made in only three patients, and was normal.
The percentage of correct diagnosis before surgery ranges from 27 to 80% with approximately 60% for infants in the other studies. In our study, 70% of the patients were correctly diagnosed, but the ratio of accurate diagnosis decreased to 50% in infants17.
According to Todani et al.6 classification, we did not encounter any intrahepatic involvement of choledochal cyst, and our patients showed homogeneity in cyst type. Only one patient with type II cyst (4%), and all others with type I cyst (96%) were seen in our series18.
The most common complications of choledochal cyst are known to be cholangitis and biliary cirrhosis in proportion to the duration and degree of obstruction before surgery and following inadequate therapy. Other complications include portal hypertension and liver abscess. We encountered 15% of cases with cholangitis related to choledochal cyst before surgery and only one infant with biliary cirrhosis. We believe that the latter patient had congenital biliary cirrhosis independent of the duration of the disease. Stones in either cyst or gallbladder are known to occur in 8-26% of the patients. We found stones in cysts or in gallbladder, or in both, in 11% of the presented cases3,19. Rupture of the cyst is generally spontaneous, but sometimes trauma may be the cause. In our study, two patients were diagnosed as spontaneous cyst rupture (8%)20. Although cystoduodenostomy was previously preferred as a surgical procedure, the high rate of complications encountered following this procedure led surgeons to find new operation methods. Internal drainage has complications of stricture formation, cholangitis, and biliary cirrhosis in approximately 50% of cases, and requires reoperation in 25% of the patients in some reports. In another report, cholangitis and choledocholithiasis occurred in 88% and 25% of cases, respectively, after cysto-enterostomy13,21. In addition, there is a remaining risk for development of cancer in the cyst wall. The reported incidence of biliary tract carcinoma in choledochal cysts varies between 2.5% and 17.5%, which is higher than that found in the general population (0.012-0.048%). Although excision of the cyst totally removes a potential risk of carcinoma, it does not exclude the possibility of the development of cancer in intrahepatic ducts. We did not see any carcinoma related to choledochal cyst to date in our series22,23. Successful treatments of choledochocele by
endoscopic sphincterectomy and transduodenal sphincterectomy with open surgery have been reported24. However, we did not perform these methods in our patients. In our series, only three patients had cystoduodenostomy; two needed reoperation for the persistence of the cysts, and the other did well. In contrast to the high rate of ascending infection reported in the literature, these three patients did not develop ascending infection after the operation.
Only one patient underwent cystojejunostomy, and was doing well two years after the operation. In older reports a 10-15% complication rate and 20% remaining risk for malignant degeneration have been estimated. However, we cannot contribute to these results because only one patient underwent cystojejunostomy25,26.
We preferred total resection of the cyst if possible and Roux-en-Y hepaticojejunostmy as a surgical procedure (n=20). We believe like others that this technique prevents most of the complications of the disease.
Peroperative liver biopsy was performed on 18 patients in our series. Despite 60% abnormal liver pathology in some reports, our records showed only two patients with periportal fibrosis and one had cirrhotic changes in the liver. This may be explained by no intrahepatic involvement in our series, and the high percentage of type IV cysts in other series1,27.
In conclusion, contrary to the general belief, choledochal cysts have no classic clinical features. USG is the major diagnostic tool, and its accuracy is increased when accompanied by MR- cholangiography and HIDA. The best surgical treatment seems to be complete excision of the cyst and Roux-en-Y hepaticojejunostomy. Choledochal cyst should be considered in the differential diagnosis of a wide spectrum of clinical features such as abdominal pain, vomiting, icterus, and abdominal mass in order to avoid lethal complications including biliary cirrhosis.
REFERENCES
- Crittenden SL, Mekinley MJ. Choledochal cyst-clinical features and classification. Am J Gastroenterol 1985; 80: 643-647.
- Cheney M, Rustad DG, Lilly JR. Choledochal cyst. World J Surg 1985; 9: 244-249.
- Robertson JF, Raine PA. Choledochal cyst: a 33-year review. Br J Surg 1988; 75: 799-801.
- Douglas AH. Case of dilatation of the common bile duct. Monthly J Med Sci 1852; 14: 97.
- Tsuchiya R, Harada N, Ito T, Furukawa M, Yashihiro J. Malignant tumors in choledochal cysts. Ann Surg 1977; 186: 22-28.
- Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts. Classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg 1977; 134: 263-269.
- Kasai M, Asakura Y, Taira Y. Surgical treatment of choledochal cysts. Ann Surg 1970; 172: 844-851.
- Stringel G, Filler RM. Fictitious pancreatitis in choledochal cyst. J Pediatr Surg 1982; 17: 359-361.
- Saing H, Tam PK, Lee JM, Nyun P. Surgical management of choledochal cysts: review of 60 cases. J Pediatr Surg 1985; 20: 443-448.
- Komi N, Takehara H, Kunitomo K. Choledochal cyst: anomalous arrangement of the pancreaticobiliary ductal system and biliary malignancy. J Gastroenterol Hepatol 1989; 4: 63-74.
- Powel CS, Sawyers JL, Reynolds VH. Management of adult choledochal cysts. Ann Surg 1981; 193: 666-667.
- Chen WJ, Chang CH, Hung WT. Congenital choledochal cyst with observations on rupture of the cyst and intrahepatic ductal dilatation. J Pediatr Surg 1973; 8: 529-538.
- Chijiiwa K, Koga A. Surgical management and long- term follow-up of patients with choledochal cysts. Am J Surg 1993; 165: 238-242.
- Couto JC, Leite JM, Machado AV, Souza NS, Silva MV. Antenatal diagnosis of a choledochal cyst. J Radiol 2002; 83: 647-649.
- Klein GMm, Frost SS. Newer imaging modalities for the preoperative diagnosis of choledochal cyst. Am J Gastroenterol 1981; 76: 148-152.
- Reuter K, Raptopoulos VD, Cantelmo N, Fitzpatrick G, Hawes LE. The diagnosis of a choledochal cyst by ultrasound. Radiology 1980; 136: 437-438.
- Yamaguchi M. Congenital choledochal cyst. Am J Surg 1980; 140: 653-657.
- Tsuchida Y, Ishida M. Dilatation of the intrahepatic ducts in congenital cystic dilatation of the common bile duct. Surgery 1971; 69: 776.
- Orenstein SR, Whitington PF. Choledochal cyst resulting in congenital cirrhosis. Am J Dis Child 1982; 136: 1025-1026.
- Karnak İ, Tanyel FC, Büyükpamukçu N, Hiçsönmez A. Spontaneous rupture of choledochal cyst: an unusual cause of acute abdomen in children. J Pediatr Surg 1997; 32: 736-738.
- Flanagan DP. Biliary cysts. Ann Surg 1975; 182: 635-643.
- Todani T, Tabuchi K, Watanabe Y, Kobayashi T. Carcinoma arising in the wall of congenital bile duct cysts. Cancer 1979; 44: 1134-1141.
- Kagawa Y, Kashihara S, Kuramoto S, Maetani S. Carcinoma arising in a congenitally dilated biliary tract. Report of a case and review of the literature. Gastroenterology 1978; 73: 1286-1294.
- Venu RP, Geenen JE, Hogan WJ, et al. Role of endoscopic retrograde cholangiopancreatography in the diagnosis and treatment of choledochocele. Gastroenterology 1984; 87: 1144-1149.
- Duckett J, Eraklis AJ, Longino L. Surgical treatment of idiopathic dilatation of common bile duct. J Pediatr Surg 1971; 6: 421.
- Ohi R, Yaoita S, Kamiyama T, Ýbrahim M, Hayashi Y, Chiba T. Surgical treatment of congenital dilatation of the bile duct with special reference to late complications after total excisional operation. J Pediatr Surg 1990; 25: 613-617.
- Shian WJ, Wang YJ, Chi CS. Choledochal cysts: a nine- year review. Acta Paediatr 1993; 82: 383-386.